Vitamin D Skin Problems in Winter: Evidence-Based Solutions for Eczema, Psoriasis and Inflammatory Skin Conditions
Introduction:
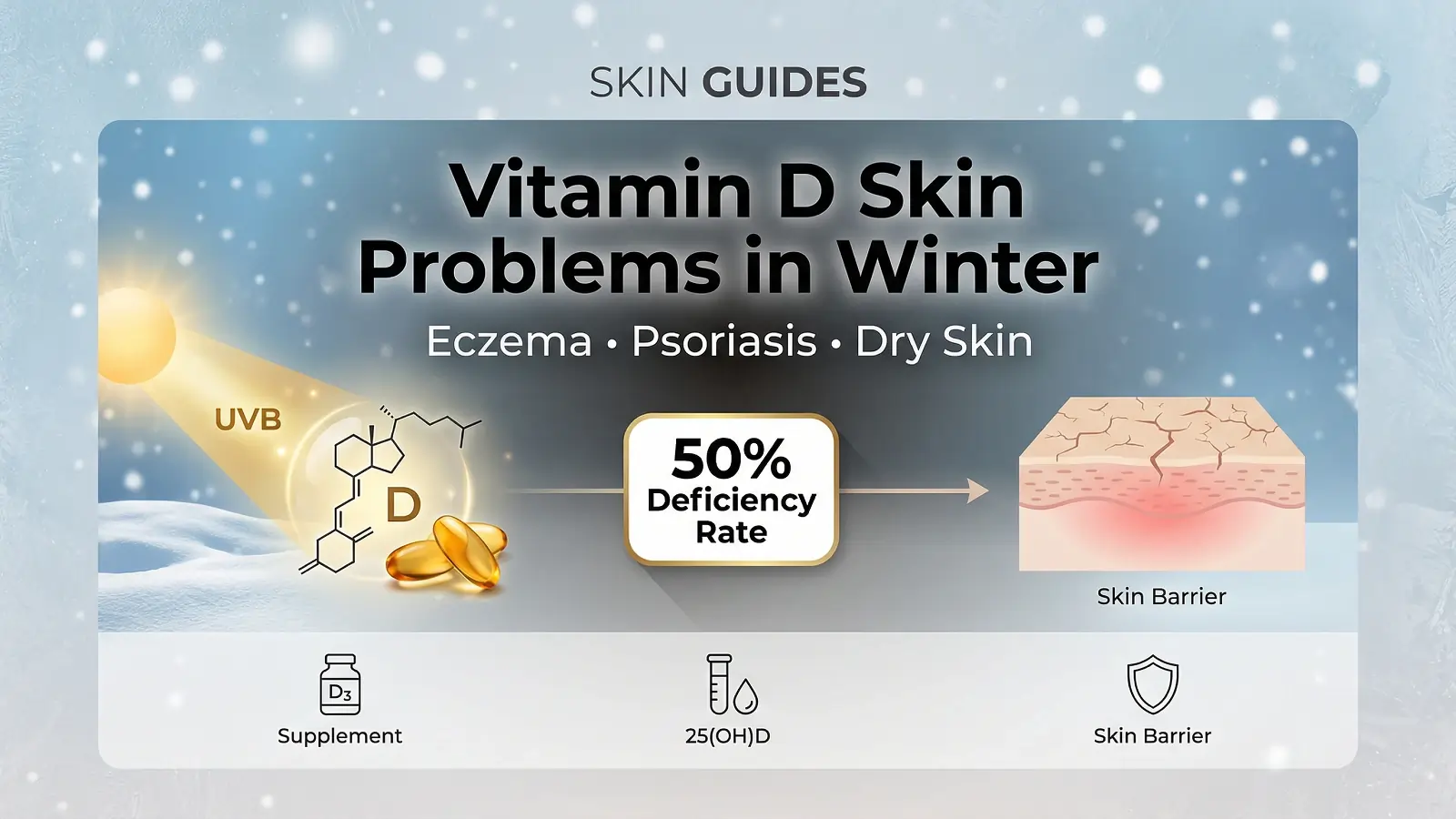
Vitamin D skin problems in winter affect at least half of the world’s population. During colder months, widespread deficiency directly impacts skin health triggering flare-ups of eczema, psoriasis, and persistent dryness that can make the season unbearable.
If you’ve noticed your skin getting progressively worse from October to March, you’re not imagining things. There’s emerging research connecting vitamin D status to winter skin conditions, revealing why your carefully maintained skincare routine suddenly fails when temperatures drop.
In this comprehensive guide, you will discover the science behind vitamin D deficiency and skin health, learn how to recognize warning symptoms, and understand evidence-based treatment protocols that can transform your winter skin. We will cover testing guidelines, supplementation strategies, and realistic timelines for improvement.
The Science Behind Vitamin D and Winter Skin Health
Understanding why winter wreaks havoc on your skin starts with comprehending how vitamin D functions as a powerful skin protector.
How Vitamin D Protects Your Skin Barrier
Your skin contains vitamin D receptors (VDR) in keratinocytes the cells making up 90% of your epidermis. When vitamin D binds to these receptors, it triggers a cascade of protective mechanisms that keep your skin healthy and resilient.
First, vitamin D stimulates the production of antimicrobial peptides, particularly cathelicidin. This natural antibiotic protects against bacterial colonization, which explains why people with vitamin D deficiency often experience increased skin infections.
Second, vitamin D regulates filaggrin production a protein essential for maintaining your skin’s barrier function. Without adequate filaggrin, your skin loses moisture rapidly and becomes susceptible to irritants and allergens.
Beyond barrier protection, vitamin D influences sebum production, collagen synthesis, and provides powerful antioxidant effects that shield against environmental damage. For a deeper understanding of how [vitamin D for skin] works at the cellular level, our comprehensive guide covers the complete mechanism. According to the National Institutes of Health Office of Dietary Supplements, vitamin D plays essential roles in numerous bodily functions beyond bone health, including immune regulation and cellular growth—both critical for skin health.
The Winter Double Whammy: Why Cold Months Devastate Skin
Winter creates the perfect storm for vitamin D skin problems. Between November and March, if you live above the 37th parallel north of San Francisco, St. Louis or Richmond UVB rays become too weak for your skin to synthesize vitamin D efficiently.
This geographical factor affects millions. Even brief outdoor exposure during winter months yields minimal vitamin D production. If you have darker skin, the situation intensifies. Higher melanin levels reduce your skin’s ability to produce vitamin D, requiring significantly longer sun exposure for equivalent synthesis.
Add indoor heating that strips humidity from the air and you have a recipe for disaster. Your already compromised skin barrier faces constant assault from dry environments while lacking the vitamin D needed for repair.
Layered winter clothing further blocks what little UVB radiation reaches your skin and disrupted circadian rhythms during shorter days interfere with natural skin repair cycles.
Key Research: The Mongolia Study That Changed Everything
Dr. Carlos Camargo’s randomized controlled trial conducted in Mongolia provided breakthrough evidence for the vitamin D-skin connection. The study followed 107 children with winter eczema, measuring outcomes using the SCORAD index a standardized assessment tool for eczema severity.
Children receiving vitamin D supplementation showed significant improvement compared to placebo groups. According to research published on PubMed, these findings suggested that vitamin D supplementation could reduce winter-related eczema severity in children with documented deficiency.
Important note: While this landmark study showed promising results, other trials have produced mixed outcomes highlighting the need for individualized treatment approaches rather than one-size-fits-all solutions.
Recognizing Vitamin D Deficiency Skin Symptoms
Identifying vitamin D skin problems in winter early can prevent months of unnecessary suffering.
Early Warning Signs on Your Skin
Your skin often reveals vitamin D deficiency before blood tests confirm it. Watch for these signals:
- Increased dryness and scaling (xerosis cutis): Skin that feels rough, flaky, and tight despite regular moisturizing
- Worsening of existing eczema patches: Previously stable areas suddenly flaring
- New onset of perioral dermatitis: Red, bumpy patches around the mouth
- Delayed wound healing: Minor cuts and scrapes taking unusually long to close
- Increased skin infections: Recurring Staphylococcus aureus colonization on affected areas
Condition-Specific Manifestations
Different skin conditions respond to vitamin D deficiency in unique ways:
Atopic Dermatitis
Presents as red, inflamed patches with intense itching. Vitamin D helps regulate the immune system and reduce the inflammatory cascade driving symptoms.
Psoriasis
Creates thicker plaques with reduced response to topical treatments. Vitamin D plays a crucial role in regulating skin cell turnover when deficient, cells reproduce too quickly, forming characteristic silvery scales.
Acne:
Shows increased inflammation and poor healing. Vitamin D calms redness and swelling while supporting tissue repair. Teenagers struggling with acne should also explore our guide on the best diet for teenagers’ skin, which covers additional nutritional strategies that complement vitamin D supplementation.
General xerosis
Manifests as cracking, flakiness, and the frustrating “winter itch” that keeps you scratching.
Systemic Symptoms Accompanying Skin Issues
Vitamin D deficiency rarely affects skin alone. Watch for these accompanying symptoms:
- Persistent fatigue and unexplained tiredness
- Bone or muscle pain, especially in legs and back
- Frequent colds and infections
- Mood changes, including depression, irritability or seasonal affective disorder
- Hair loss and brittle nails
When to Test: The 25-Hydroxyvitamin D Guidelines
The 25-hydroxyvitamin D blood test provides the most accurate assessment of your vitamin D status. For optimal skin health, aim for levels above 30 ng/mL the threshold where most skin-protective benefits become apparent.
Strategic testing timing matters. Consider scheduling tests in October (before winter’s impact) and March (at your likely lowest point) to understand your seasonal fluctuations.
Don’t simply accept “normal range” results without scrutiny. Many laboratories consider 20 ng/mL normal, but skin health often requires levels above 30-40 ng/mL for optimal function.
Evidence-Based Treatment Protocols
Once you’ve confirmed vitamin D deficiency, treatment should match your age, health status and severity of deficiency.
Age-Specific Supplementation Guidelines
Infants (0-12 months):
The American Academy of Pediatrics recommends 400-1000 IU daily for infants. Liquid D3 drops offer the easiest administration place drops directly on the nipple during breastfeeding or add to formula.
Children (1-18 years):
Weight-based dosing typically ranges from 1000-4000 IU daily. The Mongolia study achieved success with 1000 IU in children with winter eczema. Gummies appeal to picky eaters, though liquid and tablets offer more precise dosing.
Adults (19-70 years):
Standard RDA sits at 600-800 IU for most adults, though individuals with documented deficiency often need higher doses. For severe deficiency, healthcare providers may prescribe loading doses of 50,000 IU weekly for eight weeks, followed by maintenance dosing of 800-1,000 IU daily.
Always consult a healthcare provider before starting supplements.
Seniors (70+ years):
Older adults face unique challenges reduced skin synthesis capacity, age-related kidney changes affecting vitamin D conversion, and medications that may interact with supplementation. Higher doses and more frequent monitoring become essential.
Choosing the Right Vitamin D Supplement
Not all vitamin D supplements work equally. Here’s what matters:
D3 (cholecalciferol) vs. D2 (ergocalciferol): Choose D3 it’s the same type your skin produces naturally and raises blood levels more effectively.
Oil-based formulations improve absorption since vitamin D is fat-soluble. Softgels containing oil or drops suspended in MCT oil outperform dry tablets.
Quality markers include third-party testing certifications (USP, NSF, or ConsumerLab), minimal additives, and clear labeling of vitamin D content per serving.
Topical Vitamin D for Skin Conditions
Oral supplementation isn’t the only option. Topical vitamin D preparations offer direct benefits for certain conditions.
Calcipotriol 0.005% cream has demonstrated significant reductions in psoriasis severity scores through dual anti-inflammatory and antiproliferative effects. Comprehensive information from DermNet NZ confirms its effectiveness as a first-line psoriasis treatment, explaining how this vitamin D analogue works to slow skin cell production and reduce scaling.
For acne, two-month calcipotriol interventions have shown significant reductions in both inflammatory and non-inflammatory lesions.
Combination products pairing calcipotriol with betamethasone (a corticosteroid) leverage synergistic effects for enhanced results.
Vitamin D-enriched moisturizers offer gentler options for strengthening general skin barrier function without prescription requirements.
Optimizing Your Winter Skin Recovery Timeline
Managing expectations prevents frustration during treatment.
What to Expect During Treatment
Individual response varies significantly based on baseline deficiency severity, absorption capacity, and skin condition type. Studies show improvement occurring anywhere from 2 weeks to 3-6 months.
- Initial weeks: Supplementation begins; visible changes may not be apparent. Your body prioritizes internal functions before skin benefits appear.
- Weeks 3-6: Many patients report reduced itching and slight improvement in dryness. This subtle shift often provides the first encouragement.
- Weeks 6-12: Noticeable reduction in inflammation for responders. Flare intensity typically decreases before flare frequency.
- 3-6 months: Sustained improvement becomes possible with consistent supplementation. Reduced flare frequency and severity represent realistic long-term goals.
Important: Some clinical trials have shown no significant improvement even with supplementation, emphasizing the importance of working with a dermatologist for personalized treatment.
Accelerating Results: The Comprehensive Approach
Vitamin D works best as part of a multi-pronged strategy:
- Omega-3 fatty acids enhance vitamin D’s anti-inflammatory effects
- Probiotics support the gut-skin axis connection
- Optimal moisturizing routines using vitamin D-enriched products
- Humidity management targeting 40-50% indoor humidity
- Gentle cleansing protocols that don’t strip barrier oils
Monitoring and Adjusting Your Protocol
Retest vitamin D levels every 3-4 months during treatment. More frequent monitoring helps tailor dosage to individual needs and prevents overcorrection.
Watch for signs you need dosage adjustments: persistent symptoms despite supplementation, or symptoms of overcorrection like nausea, increased thirst, or confusion.
Seasonal adjustment matters. A daily dose of 800 IU may suffice in summer but often needs increasing during winter for those in northern latitudes.
Beyond Supplements: Maximizing Natural Vitamin D
Supplements provide reliable dosing, but natural sources support overall health.
Dietary Sources for Winter Months
Incorporate these vitamin D-rich foods regularly:
- Fatty fish: Salmon, mackerel, tuna, and sardines provide 400-1000 IU per serving
- Fortified dairy: Milk, kefir, yogurt, and cheese
- Plant-based alternatives: Fortified almond, soy, and oat milks
- Fortified orange juice: Check labels for vitamin D content
- Whole eggs: The yolk contains the vitamin D
- UV-exposed mushrooms: Some varieties provide meaningful amounts
- Cod liver oil: One of the most concentrated natural sources
Reality check: While these foods help, it’s often challenging to meet all vitamin D needs through diet alone especially during winter. However, following a Mediterranean diet for youthful skin naturally incorporates many vitamin D-rich foods like fatty fish and eggs while providing additional anti-inflammatory benefits.
Safe Sun Exposure in Winter
Brief, controlled sun exposure around 10-30 minutes a few times weekly is generally enough for vitamin D production without risking skin damage. Midday sun provides the strongest UVB rays, making short exposure during lunch breaks most effective. Understanding how [vitamin D protects against photoaging and UV damage] can help you balance sun exposure benefits with skin protection.
Winter reality: Research indicates that in spring and summer, 8-10 minutes around noon yields recommended levels. However, in winter, approximately two hours of noon sun exposure may be necessary when the body is covered by clothing often impractical.
Why tanning beds aren’t the answer: Both extended sun exposure and tanning beds significantly increase skin cancer risk, making them poor choices for vitamin D optimization.
UVB Lamp Option
UV lamps emitting rays similar to sunshine can help maintain or increase serum vitamin D levels. This option works particularly well for patients with fat malabsorption or those unable to meet requirements through sunlight and diet.
Use safely according to manufacturer instructions to avoid skin damage, and consider this option only after consulting with healthcare providers.
Special Populations and Considerations
Certain groups face higher risk for vitamin D skin problems in winter.
Higher Risk Groups
- Darker skin tones: Higher melanin levels significantly reduce vitamin D synthesis efficiency. Longer sun exposure is required for equivalent production compared to lighter skin.
- Obesity: Vitamin D becomes sequestered in fat tissue, reducing bioavailability despite adequate intake.
- Elderly (65+): Decreased synthesis capacity, more time spent indoors, and age-related kidney changes affecting vitamin D conversion compound risks.
- Inflammatory bowel disease and Celiac disease: Difficulty absorbing fat-soluble vitamins may require higher doses or specialized formulations.
- Kidney and liver disease: Impaired vitamin D activation may necessitate prescription calcitriol replacement beginning in stage 3 CKD.
- Gastric bypass patients: Altered digestive anatomy affects fat-soluble vitamin absorption.
Drug Interactions and Contraindications
Certain medications require careful monitoring alongside vitamin D supplementation:
- Thiazide diuretics may increase calcium levels
- Digoxin requires monitoring due to calcium interactions
- Existing hypercalcemia contraindicates high-dose supplementation
Healthcare professionals should monitor levels regularly for high-risk individuals.
Troubleshooting Common Problems
When improvement stalls, consider these factors.
When Vitamin D Isn’t Helping
Investigate other potential deficiencies zinc, vitamin A, and B vitamins all impact skin health. Absorption issues require different supplement forms or higher doses. Genetic VDR polymorphisms may reduce response to supplementation.
Important: Some individuals may not respond significantly to supplementation alone. Comprehensive treatment approaches combining multiple interventions often prove necessary.
Signs of Overcorrection
Hypercalcemia symptoms include nausea, vomiting, weakness, frequent urination and confusion. If you experience these, reduce dosage immediately and consult your healthcare provider.
Regular testing prevents overcorrection and ensures your levels remain in optimal ranges.
Frequently Asked Questions
Q: How do I know if my winter eczema is from vitamin D deficiency?
A: Common signs include increased dryness, worsening flare-ups, slow wound healing, and increased skin infections. Systemic symptoms like fatigue, bone pain, and mood changes often accompany skin manifestations. A 25-hydroxyvitamin D blood test can confirm deficiency.
Q: Can vitamin D supplements replace my prescription eczema creams?
A: No. Vitamin D supplementation works best as part of a comprehensive treatment plan alongside conventional treatments. Consult with a dermatologist for the right combination based on your specific needs.
Q: How long until I see improvement in my winter skin problems?
A: Individual response varies significantly. Some patients notice reduced itching within 3-4 weeks, while noticeable inflammation reduction may take 6-12 weeks. Full improvement may require 3-6 months of consistent supplementation.
Q: Should I take vitamin D year-round or just in winter?
A: Many people benefit from year-round supplementation with dosage adjusted seasonally. A daily dose of 800 IU may suffice in summer but may need increasing during winter, especially in northern latitudes.
Your Winter Skin Action Plan
Vitamin D skin problems in winter affect millions, but understanding the connection empowers you to take control.
Your immediate action steps:
- Schedule vitamin D level testing with your healthcare provider
- Begin appropriate supplementation based on test results and professional guidance
- Implement a comprehensive skincare routine including barrier-protective products
Allow 6-12 weeks minimum for initial assessment of treatment effectiveness. Work with healthcare providers to adjust your protocol based on results.
Disclaimer: This content is for informational purposes only and does not constitute medical advice. Always consult a healthcare provider or dermatologist before starting any supplementation regimen, especially if you have underlying health conditions or take medications.