Vitamin A Toxicity: Warning Signs You’re Taking Too Much!

Did you just realize you took too many vitamin A supplements? Maybe you’ve been enjoying liver regularly and wondering if that is a problem? Is too much vitamin A dangerous? The short answer is yes vitamin A toxicity can be scary, but it’s often manageable once you understand what’s happening in your body.
Take a breath. You are in the right place.
This comprehensive guide will help you determine whether you are at risk, recognize warning signs and know exactly what steps to take next.
📋 QUICK ANSWER
Vitamin A toxicity, also called vitamin A poisoning or hypervitaminosis A, occurs when you consume too much preformed vitamin A (retinol) typically more than 10,000 IU daily for extended periods or over 150,000 IU in a single dose. The effects of too much vitamin A include persistent headaches, nausea, dry skin, and hair loss. The reassuring news? Most cases resolve completely within weeks after stopping excessive intake. Importantly, beta-carotene from vegetables does NOT cause this condition.
What Is Vitamin A Toxicity (Hypervitaminosis A)?
Vitamin A toxicity medically termed hypervitaminosis A, vitamin A poisoning, or vitamin A intoxication is a condition caused by excessive accumulation of preformed vitamin A in your body. Unlike water-soluble vitamins that your kidneys simply flush out when you’ve had enough, vitamin A is fat-soluble. This means it gets stored in your liver and fat tissues, building up over time if you consistently consume too much.
Is too much vitamin A bad for you? Absolutely. When vitamin A accumulates beyond what your body can safely store, you can experience a range of vitamin A excess side effects that affect multiple organ systems.
The word itself tells the story: “hyper” means excess, “vitamin” refers to the nutrient, and “osis” indicates a condition. So hypervitaminosis A literally translates to “a condition of too much vitamin A.” You may also hear healthcare providers refer to this as vitamin A surplus or vitamin A intoxication.
Preformed Vitamin A vs. Provitamin A: A Critical Distinction
Understanding this difference could save you unnecessary worry or help you identify a real problem. Can too much vitamin A be toxic? Only when it comes from the preformed type.
| Type | What It Is | Where It’s Found | Can It Cause Toxicity? |
|---|---|---|---|
| Preformed Vitamin A (Retinol) | The active form your body uses directly | Liver, fish liver oils, supplements, dairy, eggs | Yes this is what causes toxicity |
| Provitamin A (Beta-Carotene) | A precursor your body converts as needed | Carrots, sweet potatoes, spinach, leafy greens | No your body regulates conversion |
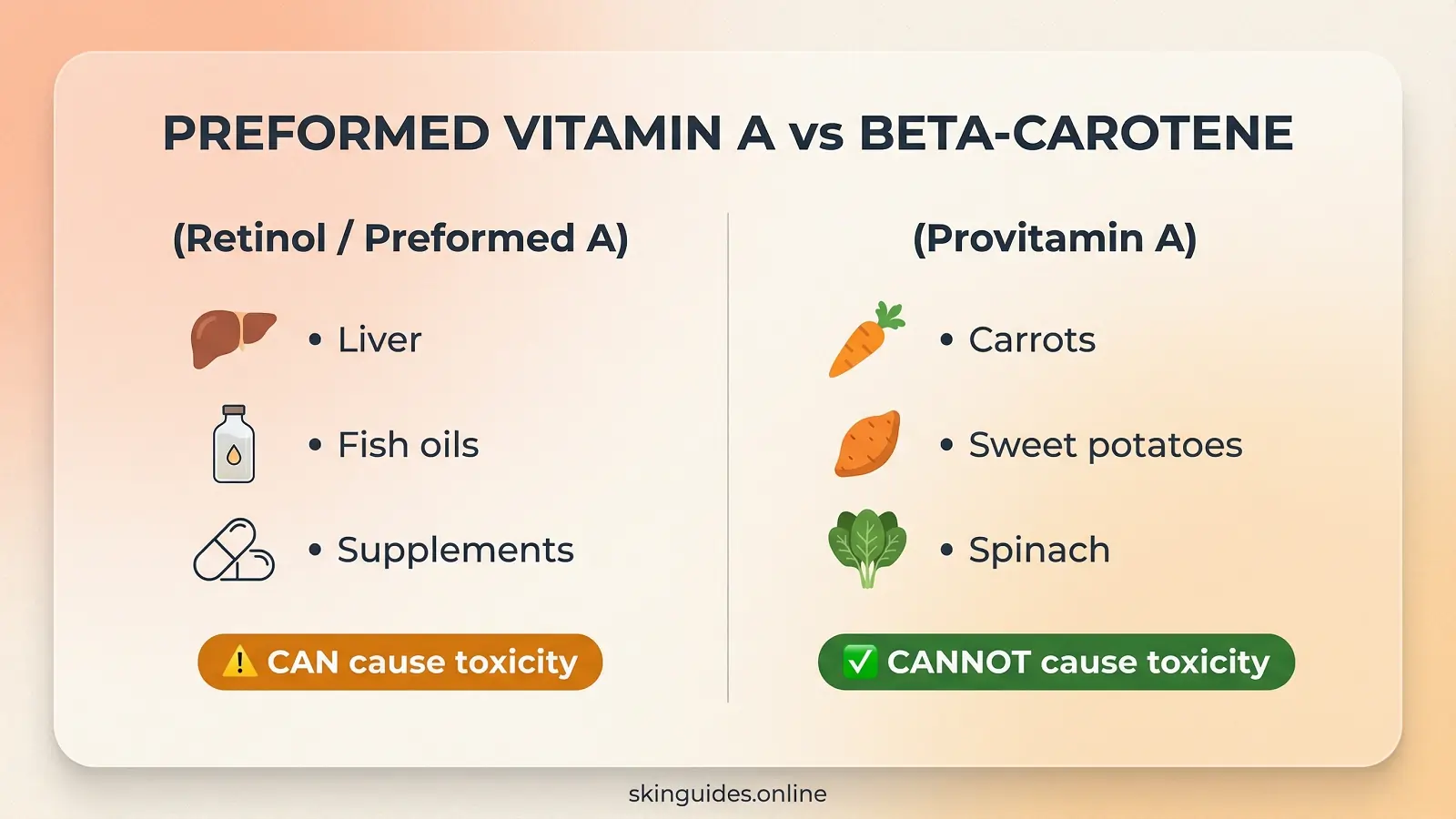
This distinction matters enormously. Is eating too much vitamin A bad when it comes from vegetables? No if you are been eating lots of carrots and your skin looks slightly orange, that is carotenemia a harmless condition where beta-carotene pigments accumulate in your skin. It’s not vitamin A toxicity and it resolves on its own.
The telltale difference? In carotenemia, the whites of your eyes stay white. In true vitamin A toxicity with liver involvement (jaundice), your eyes turn yellow.
Acute vs. Chronic Vitamin A Toxicity
Is too much vitamin A toxic? Yes, and the vitamin A overdose effects come in two distinct forms, each with different causes, symptoms and timelines.
Acute Vitamin A Toxicity
This occurs when someone ingests a very large vitamin A overdose amount in a short period typically more than 150,000 IU in adults. Think accidental overdose scenarios or, historically, Arctic explorers who consumed polar bear liver (which contains extraordinarily high vitamin A levels). When you overdose on vitamin A acutely, symptoms appear rapidly.
Symptom onset: 6 to 24 hours after ingestion
Common vitamin A intoxication symptoms include:
- Severe headache
- Nausea and vomiting
- Drowsiness and irritability
- Abdominal pain
- Blurred vision (in severe cases)
- Skin peeling (appearing 2-3 days later)
Chronic Vitamin A Toxicity
This develops gradually when someone consistently consumes more than 10,000 IU daily for months or years. Is it bad to have too much vitamin A over a long period? Definitely this is actually the more common scenario, often seen in people taking high-dose supplements without realizing the cumulative effects.
Symptom onset: Weeks to months of excessive intake
Common symptoms and side effects of too much vitamin A include:
- Persistent dry, rough, peeling skin
- Hair loss (diffuse alopecia)
- Cracked, chapped lips
- Chronic headaches
- Bone and joint pain
- Fatigue and irritability
- Loss of appetite
| Type | Dose Threshold | Onset | Recovery Time |
|---|---|---|---|
| Acute | >150,000 IU single dose | 6-24 hours | 1-2 weeks |
| Chronic | >10,000 IU/day for months | Weeks to months | 2-6 weeks (most symptoms) |
Complete Symptom Guide by Body System
Recognizing vitamin A toxicity symptoms can be tricky because the high doses of vitamin A side effects overlap with many other conditions. Here’s a comprehensive breakdown organized by body system.
Skin, Hair, and Nail Symptoms
These are often the first noticeable signs of chronic toxicity. Understanding vitamin A toxicity rash and skin manifestations is crucial for early detection:
- Dry, rough skin: Generalized dryness, especially on arms and legs
- Vitamin A toxicity rash: This typically presents as dry, scaly patches rather than a traditional raised rash the skin may appear rough, flaky, and irritated with a sandpaper-like texture. In some cases, you may notice reddened areas with significant peeling
- Peeling skin: Particularly on palms and soles a hallmark sign
- Persistent itching: Often accompanying the rash-like skin changes
- Hair loss: Diffuse thinning across the scalp (usually reversible)
- Cracked lips: Angular cheilitis or severely chapped lips
- Brittle nails: Cracking and peeling
Important Note: Hair loss caused by vitamin A toxicity is typically reversible. Most people experience complete hair regrowth within 2-6 months after stopping excessive intake.
Neurological Symptoms
These symptoms deserve particular attention because they can indicate a serious complication called increased intracranial pressure (pseudotumor cerebri).
- Persistent headache: Often worse in the morning
- Dizziness and vertigo
- Blurred or double vision
- In infants: Bulging fontanelle (soft spot) this is a medical emergency
🚨 MEDICAL ALERT:
Severe headaches combined with vision changes may indicate increased intracranial pressure. This condition mimics symptoms of a brain tumor and requires immediate medical evaluation.
Gastrointestinal and Liver Symptoms
Your liver bears the brunt of vitamin A storage and toxicity. The vitamin A overdose effects on your digestive system include:
- Nausea (especially prominent in acute overdose)
- Vomiting
- Right upper abdominal pain
- Loss of appetite
- Weight loss
- Elevated liver enzymes on blood tests
- In severe chronic cases: enlarged liver (hepatomegaly), jaundice or liver fibrosis
Important warning: Liver damage from prolonged, severe vitamin A toxicity can potentially become irreversible. This underscores why chronic high-dose supplementation without medical supervision carries genuine risks.
Bone and Joint Symptoms
Chronic excessive vitamin A intake affects your skeletal system:
- Bone pain (particularly in long bones)
- Joint pain (especially in larger joints)
- Increased fracture risk
- Decreased bone mineral density with prolonged exposure
Research published in peer-reviewed journals suggests that sustained vitamin A intakes exceeding 5,000 IU daily may increase hip fracture risk, particularly in postmenopausal women.
What Causes Vitamin A Toxicity?
Supplements: The Primary Culprit
The vast majority of vitamin A toxicity cases involve supplements, not food. Here is the reality of how people overdose on vitamin A:
| Source | Risk Level | Typical Content |
|---|---|---|
| High-dose vitamin A supplements | 🔴 High | Often 10,000-25,000 IU per capsule |
| Cod liver oil | 🟡 Moderate | 4,000-5,000 IU per tablespoon |
| Multivitamins with retinol | 🟡 Low-Moderate | Usually 2,500-3,000 IU |
| Combination supplements | 🟡 Moderate | Cumulative risk when taking multiple products |
Common question: Can a multivitamin cause vitamin A toxicity?
Standard multivitamins alone rarely cause problems. The risk increases when you’re combining them with separate vitamin A supplements, cod liver oil, or regularly eating liver.
Food Sources: Liver and Fish Oils
Can you get vitamin A toxicity from food? While it’s less common than supplement-induced toxicity, yes certain foods are concentrated enough to cause problems:
| Food | Vitamin A per Serving | Percentage of Upper Limit |
|---|---|---|
| Beef liver (3 oz) | 22,000-27,000 IU | 220-270% |
| Chicken liver (3 oz) | 11,000-14,000 IU | 110-140% |
| Cod liver oil (1 tbsp) | 4,000-5,000 IU | 40-50% |
How much liver can you eat safely? For most healthy adults, consuming liver 1-2 servings per week is generally considered safe. However, daily consumption or eating large portions regularly can easily push your intake into concerning territory, especially if you’re also taking supplements.
Can Vegetables Cause Vitamin A Toxicity?
The clear answer: No. Carrots, sweet potatoes, spinach and other beta-carotene-rich foods cannot cause vitamin A toxicity. Your body cleverly regulates how much beta-carotene it converts to active vitamin A, only producing what it needs. The worst that happens with excessive carrot consumption is temporarily orange-tinted skina harmless condition called carotenemia.
How Much Vitamin A Is Too Much?
Official Upper Limits
How much vitamin A is toxic? Here are the established thresholds:
| Age Group | Upper Limit (IU/day) | Upper Limit (mcg RAE/day) |
|---|---|---|
| Infants 0-12 months | 2,000 IU | 600 mcg |
| Children 1-3 years | 2,000 IU | 600 mcg |
| Children 4-8 years | 3,000 IU | 900 mcg |
| Children 9-13 years | 5,667 IU | 1,700 mcg |
| Teens 14-18 years | 9,333 IU | 2,800 mcg |
| Adults 19+ | 10,000 IU | 3,000 mcg |
Source: NIH Office of Dietary Supplements
Understanding IU vs. mcg Conversions
Supplement labels can be confusing. Here’s the simple conversion for preformed vitamin A:
1 IU = 0.3 mcg RAE (or conversely, 1 mcg RAE = 3.33 IU)
Note: RAE (Retinol Activity Equivalents) is the standard measurement unit
Common Dose Questions Answered
Q: Is 10,000 IU of vitamin A daily safe?
A: This is at the adult upper limit. Short-term use is generally safe, but staying at this threshold long-term isn’t recommended without medical supervision.
Is 25,000 IU of vitamin A safe?
No this exceeds the Tolerable Upper Intake Level by 150% and will likely cause toxicity symptoms if taken regularly.
I took 50,000 IU once by accident am I okay?
A single dose at this level is unlikely to cause serious harm in adults. Monitor for symptoms and avoid additional vitamin A for several days.
✅ ONE-TIME OVERDOSE REASSURANCE:
A single accidental high dose is rarely dangerous in adults. Toxicity typically requires either a massive acute dose (>150,000 IU) or chronic excessive intake over weeks to months. If you accidentally doubled or tripled your supplement dose once, stop supplementation, drink plenty of fluids and simply monitor for symptoms.
Diagnosis: What Blood Tests Show Vitamin A Toxicity?
Useful Laboratory Tests
Toxic levels of vitamin A in blood can be measured through several tests:
| Test | What It Shows | Notes |
|---|---|---|
| Serum retinol | Elevated levels suggest toxicity | Toxic levels of vitamin A typically exceed 100 mcg/dL |
| Retinyl esters | More sensitive marker for toxicity | Not commonly ordered |
| AST/ALT (liver function tests) | Liver enzyme elevation | Indicates hepatotoxicity |
| Alkaline phosphatase | May be elevated | Suggests bone/liver involvement |
| Calcium | May be elevated (hypercalcemia) | Seen in chronic toxicity |
Important note: Serum retinol levels can sometimes remain normal even when liver stores are excessive because your body tightly regulates blood levels. This is why your clinical history and symptoms are crucial for diagnosis blood tests alone may miss early or mild cases.
Vitamin A Overdose Treatment and Recovery
Step 1: Stop All Vitamin A Sources
This is the most important intervention in any vitamin A overdose treatment protocol:
✓ Discontinue vitamin A supplements immediately
✓ Stop cod liver oil and fish liver oils
✓ Review your multivitamin switch to one without retinol if needed
✓ Temporarily avoid liver and liver products
✓ Check ALL supplements for hidden vitamin A content
Step 2: Supportive Care for Mild Cases
- Stay well-hydrated
- Get adequate rest
- Track your symptoms daily
- Avoid alcohol (reduces additional liver stress)
Step 3: When to Seek Medical Care
Seek immediate care if you experience:
⚠️ Severe or worsening headache
⚠️ Vision changes (blurred or double vision)
⚠️ Persistent vomiting lasting more than 24 hours
⚠️ Jaundice (yellow skin or eyes)
⚠️ Dark urine or right upper abdominal pain
⚠️ Bulging fontanelle in an infant
⚠️ Confusion or altered mental status
⚠️ Pregnancy combined with high vitamin A exposure
Recovery Timeline: How Long Does It Take?
| Symptom | Expected Recovery Time |
|---|---|
| Nausea and GI symptoms | Days |
| Headache | 1-2 weeks |
| Dry skin and peeling | 2-4 weeks |
| Hair loss | 2-6 months for regrowth |
| Elevated liver enzymes | 2-8 weeks |
✅ GOOD NEWS:
Most vitamin A toxicity cases resolve completely once intake stops. Permanent damage is rare and typically only occurs with severe, prolonged toxicity that goes unaddressed for extended periods.
Can Topical Retinol Cause Vitamin A Toxicity?
This is a common concern, especially among skincare enthusiasts using retinol creams, serums or prescription tretinoin (Retin-A).
The answer: Extremely unlikely. Topical retinoids have minimal systemic absorption meaning very little enters your bloodstream. Vitamin A toxicity from topical retinol products has not been documented in medical literature.
However, if you are using prescription-strength retinoids like tretinoin and also taking oral vitamin A supplements, it’s worth discussing with your dermatologist to ensure you’re not creating unnecessary overlap.
Special Considerations: Pregnancy and Children
Vitamin A During Pregnancy
This deserves extra attention. Excessive preformed vitamin A during pregnancy especially in the first trimester is associated with birth defects affecting the baby’s head, heart, brain and spinal cord.
Safe limits during pregnancy:
- Upper limit: 10,000 IU/day (but many experts recommend staying under 5,000 IU/day)
- Recommended daily intake: approximately 2,565 IU
Critical actions for pregnant women:
- Verify your prenatal vitamin’s vitamin A source and amount
- Avoid additional vitamin A supplements
- Avoid liver during pregnancy (especially first trimester)
- Never take isotretinoin (Accutane) or other oral retinoids during pregnancy
- Discuss any retinoid skincare products with your doctor
Beta-carotene is safe during pregnancy and does not carry teratogenic risk. Expecting or planning pregnancy? Don’t miss my brand new complete guide that every mom-to-be is reading right now → Vitamin A During Pregnancy: Every Mom Needs to Know!
Vitamin A Toxicity in Children
Children have lower upper limits and are more vulnerable to accidental overdose from adult supplements. For complete information on proper vitamin A dosing for children, including age-specific recommendations and the best food sources, check out our dedicated guide
Warning signs in children:
- Unusual irritability
- Excessive drowsiness
- Vomiting
- Bulging fontanelle (in infants) this is an emergency
If you suspect your child has ingested excess vitamin A: Contact Poison Control immediately at 1-800-222-1222 (US) or your local emergency services.
Frequently Asked Questions
What is the first sign of vitamin A toxicity?
The first signs depend on whether you’re dealing with acute or chronic toxicity. In acute cases (large single dose), headache and nausea are typically the first symptoms to appear, usually within 6-24 hours. In chronic cases (prolonged excessive intake), dry skin and peeling skin are often the earliest noticeable signs, developing gradually over weeks to months.
Is vitamin A toxicity common?
No, vitamin A toxicity is relatively uncommon in the general population. However, it’s seen more frequently in specific groups: people taking high-dose supplements without medical supervision, those consuming liver very frequently, and individuals using multiple supplements that contain vitamin A. According to poison control center data, among supplement users taking more than 10,000 IU daily, the incidence increases significantly.
How much vitamin A is toxic?
For adults, toxic levels of vitamin A generally result from consuming more than 10,000 IU daily over extended periods (chronic toxicity) or more than 150,000 IU in a single dose (acute toxicity). The exact vitamin A overdose amount that causes symptoms varies based on individual factors like body weight, liver function, and duration of exposure. Children have much lower thresholds toxicity can occur at proportionally smaller doses.
Is too much vitamin A dangerous?
Yes, too much vitamin A is dangerous and can cause significant health problems. The vitamin A excess side effects range from uncomfortable symptoms like dry skin and headaches to serious complications including liver damage, increased intracranial pressure, and bone loss. During pregnancy, excessive vitamin A is particularly dangerous due to birth defect risks.
Can you reverse vitamin A toxicity?
Yes, absolutely. The reassuring reality is that most cases of vitamin A toxicity fully resolve after stopping excessive intake. Your body gradually processes and eliminates the stored vitamin A, and symptoms typically fade within weeks. The key is recognizing the problem and stopping the source promptly.
How long does it take to recover from vitamin A toxicity?
Recovery time varies depending on symptom severity and duration of excessive intake. Most symptoms improve significantly within 1-6 weeks after stopping vitamin A supplements. Gastrointestinal symptoms like nausea often resolve within days. Skin symptoms usually clear within 2-4 weeks. Hair regrowth, if affected, typically takes longer usually 2-6 months but hair does grow back in most cases.
Can you get vitamin A toxicity from carrots?
No, you cannot. Carrots and other orange/yellow vegetables contain beta-carotene (provitamin A), not preformed vitamin A. Your body intelligently regulates how much beta-carotene it converts to active vitamin A it only makes what it needs. Can you get vitamin A toxicity from food? Only from animal sources like liver, not from plant-based foods.
Can you get vitamin A toxicity from food?
Yes, but it’s uncommon. Vitamin A toxicity from food primarily occurs with frequent consumption of liver, which contains extremely high concentrations of preformed vitamin A. A single serving of beef liver contains 2-3 times the daily upper limit. Regular liver consumption, especially combined with supplements, can lead to toxicity. Plant foods containing beta-carotene cannot cause toxicity.
Is 10,000 IU of vitamin A daily safe?
It’s at the upper limit proceed with caution. For most healthy adults, 10,000 IU daily is at the threshold established as the Tolerable Upper Intake Level. Short-term use is generally safe, but long-term daily consumption at this level requires caution, especially for pregnant women, people with liver conditions, and older adults. If you are taking this amount regularly, consider discussing it with your healthcare provider.
Does vitamin A toxicity cause permanent damage?
Rarely. The majority of vitamin A toxicity cases resolve completely without lasting effects. However, permanent damage can occur in severe, prolonged cases particularly with significant liver involvement (fibrosis or cirrhosis) or untreated pseudotumor cerebri (which can affect vision). Early recognition and stopping excessive intake prevents permanent complications in nearly all cases.
What blood test shows vitamin A toxicity?
Several blood tests can help diagnose vitamin A toxicity. Serum retinol levels above 100 mcg/dL are suspicious for toxicity these are considered toxic levels of vitamin A. Retinyl esters are a more sensitive marker but aren’t commonly ordered. Liver function tests (AST, ALT) may show elevation indicating hepatotoxicity. However, blood tests can sometimes be normal in early cases, so clinical history and symptoms remain crucial for diagnosis.
Can topical retinol cause vitamin A toxicity?
Extremely unlikely. Topical retinol creams, serums and even prescription tretinoin (Retin-A) have minimal systemic absorption. The amount that enters your bloodstream is negligible compared to oral supplements. There are no documented cases of vitamin A toxicity from topical retinoid use alone. These products are considered safe when used as directed.
How much liver can I eat safely?
For most healthy adults, 1-2 servings of liver per week is generally considered safe. Liver is extraordinarily nutrient-dense, with a single 3-ounce serving of beef liver containing 22,000-27,000 IU of vitamin A more than double the daily upper limit. Daily consumption or large portions can quickly push you into toxicity territory, especially if combined with supplements.
Should I avoid vitamin A completely?
Absolutely not! Vitamin A is an essential nutrient crucial for vision, immune function, skin health, and reproduction. Your body needs it to function properly. The goal isn’t elimination it’s staying within safe limits. Most people get adequate vitamin A from a balanced diet without supplementation. If you do supplement, choose moderate doses and be aware of your total intake from all sources.
Key Takeaways
✅ Vitamin A toxicity (vitamin A poisoning) comes from retinol (preformed vitamin A), not beta-carotene from vegetables
✅ The adult upper limit is 10,000 IU daily exceeding this chronically increases toxicity risk
✅ First signs include headache and nausea (acute) or dry/peeling skin and vitamin A toxicity rash (chronic)
✅ Vitamin A overdose treatment is straightforward: stop the source, and symptoms typically resolve within weeks
✅ Most cases are fully reversible permanent damage is rare with prompt intervention
✅ Is vitamin A toxicity common? No, but it occurs more frequently in supplement users
✅ Pregnancy requires extra caution due to birth defect risks
✅ Topical retinol is safe minimal systemic absorption means no toxicity risk
✅ One-time overdose is usually not dangerous monitor symptoms and stay hydrated
✅ Don’t avoid vitamin A entirely it’s essential; just stay within safe limits
✅ Seek medical care for severe headache, vision changes or persistent vomiting
Conclusion
Vitamin A toxicity, also known as vitamin A poisoning, while potentially serious, is a manageable and usually reversible condition when caught early. The most important takeaway from this guide is that knowledge is your best protection. Understanding the difference between preformed vitamin A (which can cause toxicity) and beta-carotene (which cannot) immediately eliminates unnecessary worry for many people.
Is too much vitamin A bad for you? Yes but the good news is that vitamin A overdose treatment is usually straightforward. If you’re currently experiencing symptoms that might be related to vitamin A toxicity, the first and most critical step is simple: stop all vitamin A supplements and high-dose sources immediately. Most people see significant improvement within weeks, and complete recovery is the norm rather than the exception.
Remember that vitamin A itself is not the enemy it is an essential nutrient your body genuinely needs. The goal isn’t avoidance but rather informed, moderate consumption that supports your health without crossing into excess.
Your health is worth the attention and understanding vitamin A toxicity puts you in control.
Disclaimer: This article provides educational information and should not replace professional medical advice. Always consult qualified healthcare providers for personal health decisions.