How Vitamin D Protects Against Photoaging and UV Damage: The Complete Scientific Guide
Introduction
While we’ve been told to avoid the sun to prevent aging, new research reveals a fascinating paradox: vitamin D protects against photoaging and UV damage in ways scientists are only beginning to fully understand. The very compound produced during sun exposure may actually be one of our skin’s most powerful defenders against premature skin aging.
This seemingly contradictory finding has reshaped how dermatologists and skincare experts approach sun protection strategies. Ultraviolet radiation undeniably induces DNA damage, oxidative stress, inflammatory reactions and degradation of extracellular matrix proteins all contributing to the aged skin phenotype we associate with excessive sun exposure. Yet the very mechanism that makes sunlight potentially harmful also triggers our body’s production of a remarkably protective compound.
Understanding this vitamin D paradox in photoprotection opens doors to smarter skincare strategies. Rather than choosing between sun avoidance and vitamin D benefits, emerging science suggests we can optimize both. Throughout this comprehensive guide, you will discover how vitamin D shields your skin at the molecular level, what clinical research reveals about its protective effects, and practical strategies for harnessing these benefits while minimizing UV damage.
This guide synthesizes findings from peer-reviewed dermatological research, clinical trials and molecular biology studies to provide you with evidence-based information you can actually use.
Whether you are concerned about preventing future photoaging or addressing existing sun damage, the science of vitamin D offers promising insights. For a complete understanding of how vitamin D benefits your skin beyond photoaging including its role in treating acne, eczema, psoriasis and deficiency symptoms explore our comprehensive guide.
Understanding Photoaging and UV Damage
The Science of Photoaging
Photoaging differs fundamentally from chronological aging. While both processes cause skin changes over time, photoaging results specifically from cumulative UV exposure and produces distinct characteristics that dermatologists can readily identify.
“When UVB radiation penetrates your skin, it gets absorbed by DNA and RNA, triggering the formation of cyclobutane pyrimidine dimers (CPDs) and other damaging photoproducts. According to the Skin Cancer Foundation, these molecular changes initiate a cascade of events that accelerate skin aging far beyond what your genetic clock would naturally dictate”
The visible timeline of photoaging follows a predictable pattern. In your twenties, subtle changes begin accumulating beneath the surface. By your thirties and forties, fine lines and uneven pigmentation emerge. Without intervention, the fifties and beyond bring deeper wrinkles, solar elastosis (the leathery texture of severely sun-damaged skin), and pronounced pigmentation irregularities.
Key markers that distinguish photoaged skin include:
- irregular pigmentation
- coarse wrinkles
- loss of elasticity
- the characteristic yellowed, thickened appearance of solar elastosis
These changes occur predominantly on sun-exposed areas face, neck, hands and forearms creating a stark contrast with protected skin.
Cellular Mechanisms of UV Damage
Understanding how UV radiation damages skin cells reveals why vitamin D’s protective mechanisms prove so valuable. The damage occurs through multiple interconnected pathways.
DNA damage represents the most direct form of UV injury. CPDs and 6-4 photoproducts distort DNA structure, potentially causing mutations if not properly repaired. Upon UV exposure, mechanisms involving:
- DNA damage
- oxidative stress
- inflammation
- apoptosis
- ECM remodeling
- collagen degradation
- immune suppression
work together to cause premature aging.
Oxidative stress amplifies the damage significantly. UV radiation generates reactive oxygen species (ROS) that attack cellular components indiscriminately. These free radicals damage proteins, lipids, and additional DNA sites, creating a chain reaction of cellular injury.
Matrix metalloproteinases (MMPs) activate in response to UV exposure, breaking down collagen and elastin—the structural proteins that keep skin firm and resilient. This ECM degradation directly causes wrinkles and sagging.
The inflammatory cascade compounds all other damage types. UV-triggered inflammation releases cytokines and other mediators that perpetuate tissue destruction long after the initial exposure ends.
The Cumulative Nature of Photodamage
Prevention proves far more effective than reversal because photodamage accumulates silently for years before becoming visible. Each unprotected sun exposure adds to your lifetime UV burden, causing subclinical damage that compounds over time.
Repeated sub-erythemal exposures doses below the threshold for visible sunburn—still inflict significant cellular damage. This silent accumulation explains why photoaging often seems to appear suddenly after decades of gradual buildup.
The Vitamin D-Skin Connection
Vitamin D Synthesis in Skin
Your skin serves as a remarkable vitamin D factory. As explained by the National Institutes of Health Office of Dietary Supplements, one important human benefit of exposure to terrestrial solar UVB radiation (approximately 295 to 315 nm) is the cutaneous synthesis of vitamin D3, initiated by the photoconversion of 7-dehydrocholesterol to previtamin D3.
This synthesis pathway transforms cholesterol precursors in your skin into the hormone precursor that affects virtually every tissue in your body. The conversion requires UVB wavelengths specifically window glass blocks these wavelengths, which explains why you can’t synthesize vitamin D through closed windows.
This UVB dependency also explains why [vitamin D skin problems in winter] become so prevalent; between November and March, UVB rays above the 37th parallel become too weak for adequate synthesis, triggering eczema flare-ups, psoriasis worsening, and persistent dryness.
Beyond the classic vitamin D pathway, your skin contains additional enzyme systems that create protective metabolites locally. CYP27B1 and CYP11A1 pathways in skin cells produce active vitamin D forms right where UV damage occurs, providing immediate local protection independent of systemic vitamin D levels.
Vitamin D Receptors in Skin Cells
Vitamin D receptors (VDR) exist throughout your skin in keratinocytes, fibroblasts and melanocytes alike. These receptors allow vitamin D to directly influence skin cell behavior at the genetic level.
When activated, VDRs function as nuclear receptors that regulate gene transcription. The effects achieved through VDR activation include:
- immunomodulation
- anti-inflammatory actions
- regulation of keratinocyte proliferation and differentiation programs that build the epidermal barrier necessary to maintain skin homeostasis
This widespread receptor distribution means vitamin D can orchestrate protective responses throughout all skin layers, coordinating defense mechanisms across different cell types simultaneously.
Active Metabolites and Their Roles
While 1,25(OH)2D3 (calcitriol) represents the primary active form of vitamin D, researchers have identified numerous other metabolites with significant biological activity. Novel CYP11A1-derived metabolites show particular promise for skin protection.
Lumisterol derivatives—produced when previtamin D3 undergoes alternative conversion pathways also demonstrate protective functions. These varied metabolites provide redundant protection mechanisms, ensuring skin cells have multiple defensive tools available.
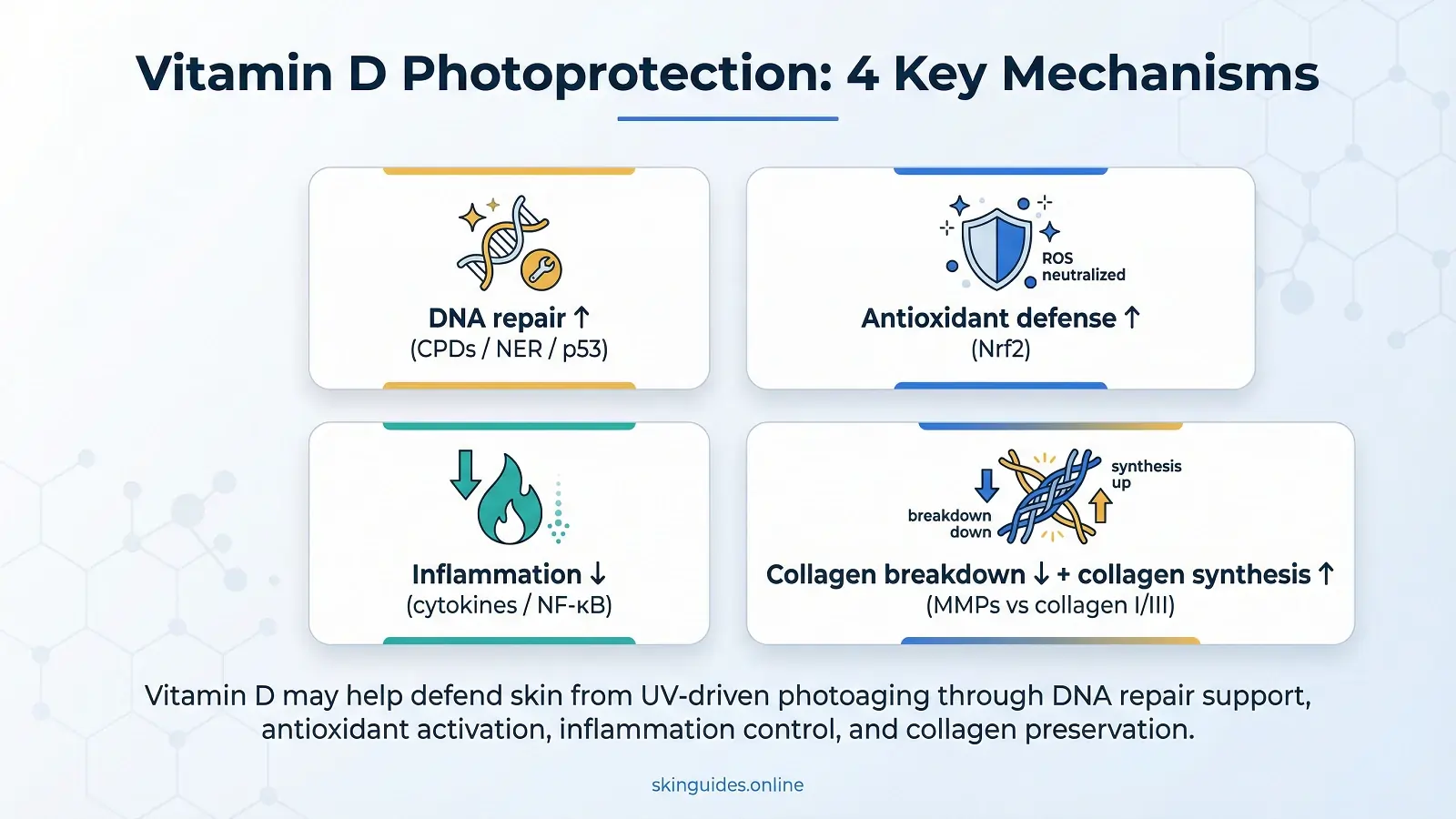
Molecular Mechanisms of Vitamin D Protection
DNA Repair Enhancement
Perhaps the most critical way vitamin D protects against photoaging involves enhancing your skin’s ability to repair UV-induced DNA damage.
Vitamin D3 protects the skin against photoaging by regulating p53-mediated pathways. The tumor suppressor protein p53 activates upon UV exposure to control cellular responses to DNA damage. Activation of p53 enhances nucleotide excision repair and promotes G1 phase cell cycle arrest, allowing time to repair damaged DNA before replication.
The nucleotide excision repair (NER) pathway, which specifically removes CPDs and 6-4 photoproducts, receives direct upregulation from vitamin D signaling. XPC protein a critical component of damage recognition in NER—increases in vitamin D-treated cells.
This enhanced repair capacity means UV-induced mutations get corrected more efficiently, reducing the cumulative damage that causes photoaging and potentially skin cancer.
Antioxidant Defense via Nrf2 Pathway
Vitamin D activates one of the body’s most powerful antioxidant response systems the Nrf2 pathway.
Research demonstrates that pretreatment of keratinocytes with 1,25(OH)2D3 or CYP11A1-derived vitamin D3 or lumisterol hydroxy-derivatives protected them against UVB-induced damage via activation of the Nrf2-dependent antioxidant response and p53-phosphorylation.
The mechanism involves 1,25(OH)2D3 exerting an antioxidant role by transcriptional regulation of Nrf2 via the vitamin D receptor. When activated, Nrf2 dissociates from its inhibitor Keap1 and travels to the cell nucleus, where it switches on genes for protective enzymes.
These enzymes include:
- glutathione (GSH)
- catalase
- superoxide dismutase (SOD)
- metallothionein
Together, they neutralize reactive oxygen species before they can damage cellular components. Vitamin D also provides mitochondrial protection, shielding these cellular powerhouses from oxidative injury.
Anti-Inflammatory Actions
Chronic inflammation drives many photoaging processes, making vitamin D’s anti-inflammatory properties particularly valuable.
Calcitriol counteracts the inflammatory responses to UV photodamage by:
- suppressing inflammatory cytokines such as TNF, IL-1, interferon-gamma, and IL-2a
- enhancing anti-inflammatory cytokines IL-4 and IL-10
This dual action reducing pro-inflammatory signals while boosting anti-inflammatory ones creates comprehensive inflammation control.
NF-κB pathway suppression represents a key mechanism, as this transcription factor controls expression of numerous inflammatory genes. By modulating cytokine production, vitamin D prevents the chronic low-grade inflammation that accelerates skin aging.
Collagen Preservation and Synthesis
Maintaining collagen the protein responsible for skin’s structural integrity proves essential for preventing photoaging’s characteristic wrinkles and sagging.
Research shows that vitamin D treatment leads to significant increases in collagen production. Day 5 cell culture supernatants showed a significant per cell increase in collagen type I and type III as measured by ELISA. Both collagen types contribute to skin firmness and resilience.
Beyond stimulating new collagen synthesis, vitamin D inhibits matrix metalloproteinases the enzymes that break down existing collagen. This dual action preserves extracellular matrix integrity, preventing the solar elastosis characteristic of severe photoaging.
Clinical Evidence and Research Findings
Human Studies on Vitamin D and Photoaging
Clinical research increasingly supports vitamin D’s photoprotective benefits in real-world conditions.
Studies demonstrate that the oral administration of high-dose vitamin D3 shortly after UVB exposure could reverse rapidly the photo-induced cutaneous damage by decreasing inflammation and inducing repair mechanisms of the epidermal barrier. This finding suggests vitamin D may help address acute sun damage when taken promptly.
Clinical trials measuring biomarkers of photoaging show improvements in participants optimizing their vitamin D status. Visual aging assessments correlate with these molecular improvements, demonstrating real-world benefits visible to both clinicians and patients.
Comparative Studies: Oral vs Topical Application
Both oral supplementation and topical application offer benefits, though they work through somewhat different mechanisms.
Research into topical formulations reveals that the average skin retention of vitamin D3 liposomes was 1.65 times that of vitamin D3 solution. Vitamin D3 liposomes could repair the surface morphology of skin in the photoaging model and promote the production of new collagen fibers.
Liposomal formulations show particular promise due to enhanced absorption and bioavailability. The ability to deliver vitamin D directly to affected skin areas provides concentrated local effects that oral supplementation may not achieve as effectively.
ose-Response Relationships
Optimal serum vitamin D levels for photoprotection appear to fall between 40-60 ng/ml somewhat higher than levels considered adequate for bone health alone. Therapeutic dosing for addressing existing damage typically exceeds preventive maintenance doses.
Safety margins remain wide, with toxicity concerns arising only at extremely high intake levels. However, individual variation in response makes professional guidance valuable for optimization.
Practical Application Strategies
Optimizing Vitamin D Status
Achieving optimal vitamin D status requires a multi-faceted approach. Regular testing through 25(OH)D blood tests establishes your baseline and monitors progress. According to guidelines from the Endocrine Society, target ranges of 40-60 ng/ml provide meaningful photoprotection beyond basic adequacy levels.
Supplementation offers the most reliable way to achieve and maintain optimal levels, particularly for those with limited sun exposure or darker skin tones. Vitamin D3 (cholecalciferol) demonstrates superior efficacy compared to D2 (ergocalciferol) for raising serum levels.
Dietary sources
- fatty fish
- fortified foods
- egg yolks
It contribute meaningfully but rarely suffice alone for achieving photoprotective levels. However, combining vitamin D-rich foods with a comprehensive anti-aging diet for skin creates a synergistic nutritional approach that addresses multiple photoaging pathways simultaneously, from collagen support to antioxidant defense.
Balancing Sun Exposure and Protection
Smart sun exposure strategies can provide vitamin D benefits while limiting damage. Research demonstrates that using SPF 17, participants were able to increase >7 nmol/L of vitamin D levels while preventing the development of actinic keratoses. This finding contradicts concerns that sunscreen completely blocks vitamin D synthesis.
The prevailing studies show that people who use sunscreen daily can maintain their vitamin D levels. Brief unprotected exposure during non-peak hours, combined with consistent sunscreen use during extended outdoor time, balances competing needs effectively.
Topical Vitamin D Applications
Topical vitamin D formulations offer targeted skin benefits. Various derivatives and analog forms provide options for different skin types and concerns. Application protocols typically involve evening use, as vitamin D compounds can degrade with UV exposure.
Combining topical vitamin D with complementary actives particularly antioxidants like vitamins C and E may enhance overall photoprotective effects. Our detailed guide on vitamin C for mature aging skin explains how this powerful antioxidant works synergistically with vitamin D to neutralize free radicals, boost collagen synthesis, and provide comprehensive protection against UV-induced aging. Retinoid compatibility requires attention, as both compounds affect similar cellular pathways.
Part 6: Safety Considerations and Contraindications
Potential Risks and Side Effects
While vitamin D toxicity remains rare, hypercalcemia can occur with extremely high supplementation doses. Symptoms include:
- nausea
- weakness
- kidney problems
Drug interactions warrant attention, particularly with certain heart medications and steroids.
Monitoring and Adjustment
Regular serum testing typically every 3-6 months during optimization, then annually for maintenance ensures appropriate levels without excess. Professional consultation becomes essential for those with kidney disease, granulomatous conditions or other medical complexities.
Frequently Asked Question
Q: Can vitamin D reverse existing sun damage?
Research suggests vitamin D can help repair recent UV damage and may gradually improve some existing photoaging signs through enhanced cellular repair mechanisms.
Q: Does darker skin need different vitamin D approaches?
Yes higher melanin levels reduce vitamin D synthesis efficiency, often requiring higher supplementation doses to achieve optimal levels.
Q: What’s the difference between vitamin D2 and D3 for skin health?
Vitamin D3 more effectively raises and maintains serum levels, making it the preferred form for photoprotection purposes.
Q: How do I know if my vitamin D levels are optimal for skin protection?
Blood testing for 25(OH)D remains the only reliable method; target levels between 40-60 ng/ml for photoprotective benefits.
Conclusion
The evidence clearly demonstrates that vitamin D can counteract the adverse effects of photo-damage by enhancing DNA repair systems, removal of ROS, anti-inflammation, and immunomodulation. This multi-pathway protection makes vitamin D a valuable component of comprehensive photoaging prevention.
Practical implementation involves optimizing your vitamin D status through appropriate supplementation, considering topical applications, and balancing smart sun exposure with consistent protection. Rather than viewing sun exposure and photoaging prevention as incompatible goals, understanding vitamin D’s role reveals sophisticated strategies for achieving both.
Disclaimer
This information is provided for educational purposes only and does not constitute medical advice. Individual responses to vitamin D vary significantly based on genetics, health status and other factors. Always consult qualified healthcare professionals before beginning any supplementation program. Evidence regarding vitamin D and photoaging continues evolving as research progresses.